The SOAP note is a widely used method of documenting patient information in a clear and organized manner. Developed by Dr. Lawrence Weed in the 1960s, the SOAP note stands for Subjective, Objective, Assessment, and Plan, providing a structured approach to clinical documentation. This method is crucial for healthcare professionals as it ensures that all relevant information is captured and communicated effectively among the healthcare team, contributing to better patient outcomes.
Understanding the SOAP Note Structure

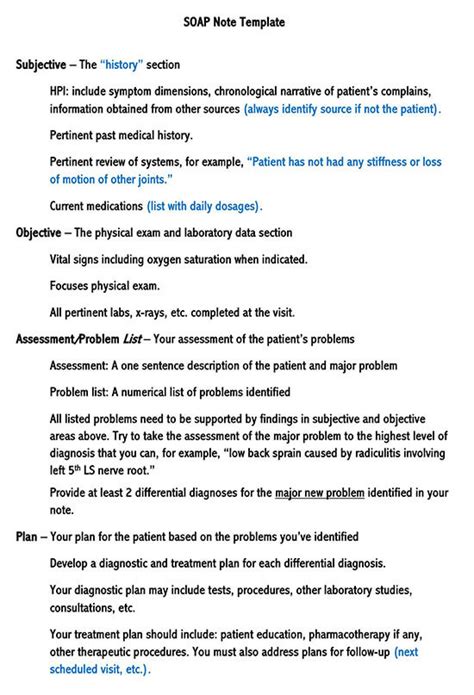
The SOAP note is divided into four main sections, each serving a distinct purpose in the documentation process.
Subjective Section
The subjective section contains information provided by the patient, including their chief complaint, history of present illness, past medical history, family history, social history, and a review of systems. This section is essential for understanding the patient’s perspective on their condition and for identifying any symptoms or concerns they may have. For instance, in a SOAP note for a patient presenting with respiratory symptoms, the subjective section might include details about the onset of symptoms, any exacerbating or relieving factors, and how the symptoms have affected the patient’s daily life.
Objective Section
The objective section includes information that can be measured or observed by the healthcare provider, such as vital signs, physical examination findings, laboratory results, and imaging studies. This section provides quantitative data that can help in assessing the patient’s condition objectively. For example, in the case of a patient with respiratory symptoms, the objective section might detail the patient’s oxygen saturation, respiratory rate, and any abnormal findings on lung auscultation.
Assessment Section
The assessment section is where the healthcare provider synthesizes the information from the subjective and objective sections to formulate a diagnosis or a list of potential diagnoses. This section may also include the provider’s impression of the patient’s condition, based on the information gathered. For a patient presenting with respiratory symptoms, the assessment might include a diagnosis of acute bronchitis or pneumonia, along with any contributing factors or comorbid conditions that could influence the treatment plan.
Plan Section
The plan section outlines the actions to be taken to address the patient’s condition, including any treatments, medications, lifestyle modifications, or further diagnostic testing that may be necessary. This section should be detailed enough to guide other healthcare professionals in the patient’s care. For instance, the plan for a patient diagnosed with acute bronchitis might include a prescription for an antibiotic, instructions for rest and hydration, and a recommendation for follow-up to assess the response to treatment.
| SOAP Note Component | Example Content |
|---|---|
| Subjective | Patient reports a 3-day history of cough and fever |
| Objective | Vital signs: Temperature 38.5°C, Respiratory rate 24/min, Oxygen saturation 92% on room air |
| Assessment | Diagnosis: Acute bronchitis |
| Plan | Patient to receive azithromycin 250mg PO daily for 5 days, and to follow up in the clinic in 1 week |
Key Points
- The SOAP note is a standardized method for documenting patient information, making it easier for healthcare providers to communicate effectively.
- The subjective section captures the patient's reported symptoms and medical history.
- The objective section includes measurable data such as vital signs and laboratory results.
- The assessment section synthesizes the information to formulate a diagnosis.
- The plan section outlines the treatment strategy and any necessary follow-up actions.
By adhering to the SOAP note structure, healthcare professionals can ensure that patient care is well-documented, and that all relevant information is readily available to inform treatment decisions. This approach contributes to more efficient and effective care, ultimately leading to better patient outcomes.
What is the primary purpose of the SOAP note in healthcare documentation?
+The primary purpose of the SOAP note is to provide a standardized and structured approach to documenting patient information, facilitating clear and effective communication among healthcare providers.
How does the SOAP note contribute to patient care?
+The SOAP note contributes to patient care by ensuring that all relevant information is captured and communicated effectively among the healthcare team, leading to more accurate diagnoses and more effective treatment plans.
What are the four main sections of a SOAP note?
+The four main sections of a SOAP note are Subjective, Objective, Assessment, and Plan, each serving a distinct purpose in the documentation and care process.
In conclusion, the SOAP note is an indispensable tool in healthcare, offering a structured framework for patient documentation. Its utility extends beyond mere documentation, playing a pivotal role in enhancing patient care through improved communication and documentation. As healthcare continues to evolve, the importance of the SOAP note in maintaining high standards of care and facilitating effective communication among healthcare providers will only continue to grow.



