Molina Healthcare is a health insurance organization that provides a range of services to its members, including prior authorization for certain medical procedures and medications. Prior authorization is a process where healthcare providers must obtain approval from the insurance company before performing a specific treatment or prescribing a particular medication. This process helps ensure that the treatment or medication is medically necessary and covered under the patient's insurance plan.
Understanding the Molina Healthcare Prior Authorization Form
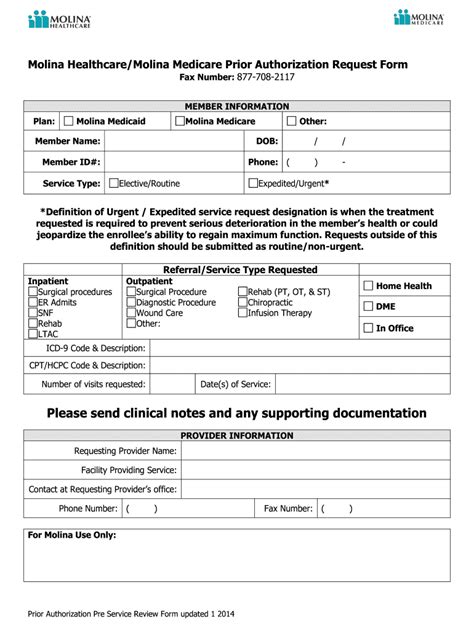
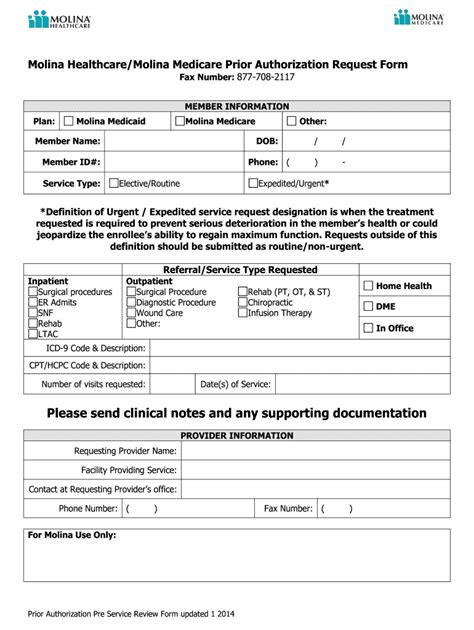
The Molina Healthcare prior authorization form is a document that healthcare providers must complete and submit to Molina Healthcare for review and approval. The form typically requires information about the patient, the treatment or medication being requested, and the medical reason for the request. Healthcare providers must fill out the form accurately and completely to ensure that the request is processed efficiently and effectively.
Required Information for the Prior Authorization Form
The Molina Healthcare prior authorization form requires the following information:
- Patient demographics, including name, date of birth, and member ID number
- Provider information, including name, address, and contact details
- Treatment or medication being requested, including dosage and frequency
- Medical reason for the request, including diagnosis and relevant medical history
- Supporting documentation, such as medical records and test results
| Required Field | Description |
|---|---|
| Patient Name | The patient's full name as it appears on their insurance card |
| Member ID Number | The patient's unique member ID number assigned by Molina Healthcare |
| Provider Name | The name of the healthcare provider requesting prior authorization |
| Treatment or Medication | The specific treatment or medication being requested, including dosage and frequency |
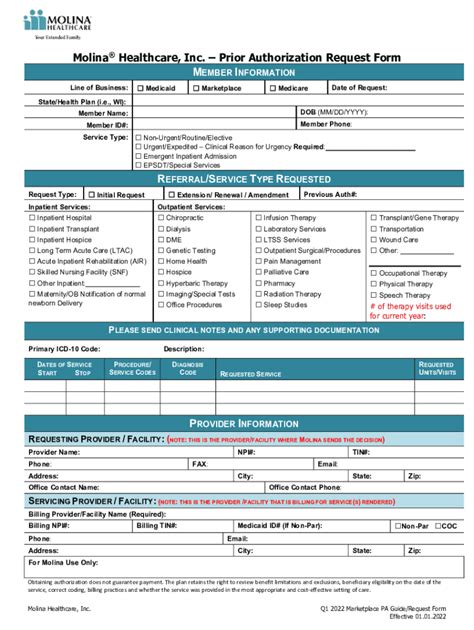
Submitting the Prior Authorization Form
Once the prior authorization form is completed, healthcare providers can submit it to Molina Healthcare via fax, mail, or online portal. The submission process typically involves the following steps:
- Completing the prior authorization form with all required information
- Attaching supporting documentation, such as medical records and test results
- Submitting the form and supporting documentation to Molina Healthcare via the preferred method
- Receiving a response from Molina Healthcare regarding the prior authorization request
Key Points
- The Molina Healthcare prior authorization form requires accurate and complete information to ensure efficient processing
- Healthcare providers must submit the form and supporting documentation to Molina Healthcare via the preferred method
- Prior authorization is required for certain medical procedures and medications to ensure medical necessity and coverage under the patient's insurance plan
- Delays or denials can occur if the prior authorization form is incomplete or inaccurate
- Healthcare providers should ensure timely submission of the prior authorization form to avoid delays in patient care
Prior Authorization Form Guidelines
To ensure efficient processing of the prior authorization form, healthcare providers should follow these guidelines:
1. Complete the form accurately and thoroughly, including all required information.
2. Attach supporting documentation, such as medical records and test results, to the form.
3. Submit the form and supporting documentation to Molina Healthcare via the preferred method.
4. Allow sufficient time for Molina Healthcare to review and respond to the prior authorization request.
| Submission Method | Contact Information |
|---|---|
| Fax | (877) 823-7346 |
| Molina Healthcare, Attn: Prior Authorization, PO Box 4042, Long Beach, CA 90801 | |
| Online Portal | https://www.molinahealthcare.com/providers/prior-authorization |
What is the purpose of the Molina Healthcare prior authorization form?
+The Molina Healthcare prior authorization form is used to request approval for certain medical procedures and medications. It helps ensure that the treatment or medication is medically necessary and covered under the patient’s insurance plan.
How do I submit the prior authorization form to Molina Healthcare?
+The prior authorization form can be submitted to Molina Healthcare via fax, mail, or online portal. The submission process typically involves completing the form with all required information, attaching supporting documentation, and submitting it to Molina Healthcare via the preferred method.
What happens if the prior authorization form is incomplete or inaccurate?
+If the prior authorization form is incomplete or inaccurate, it may result in delays or denials. Healthcare providers should ensure that the form is completed accurately and thoroughly to avoid delays in patient care.