Molina Healthcare has been a prominent player in the Medicaid landscape, providing comprehensive healthcare services to low-income individuals and families across the United States. With a rich history spanning over three decades, Molina Healthcare has established itself as a trusted and reliable Medicaid provider, with a strong commitment to delivering high-quality, patient-centered care. As of 2022, Molina Healthcare serves approximately 4.8 million Medicaid members, with a network of over 350,000 healthcare providers across 14 states, including California, Florida, Illinois, Michigan, New Mexico, New York, Ohio, Puerto Rico, Texas, Utah, Washington, and Wisconsin.
Medicaid Expansion and Molina Healthcare
The Affordable Care Act (ACA) of 2010 brought about significant changes to the Medicaid program, including the expansion of eligibility to more low-income individuals and families. Molina Healthcare has been at the forefront of this expansion, working closely with state governments to implement Medicaid expansion and provide coverage to millions of newly eligible individuals. According to a report by the Kaiser Family Foundation, as of 2022, 38 states and the District of Columbia have expanded their Medicaid programs, with Molina Healthcare playing a significant role in several of these states. For instance, in California, Molina Healthcare has partnered with the state to provide Medicaid coverage to over 900,000 low-income individuals and families.
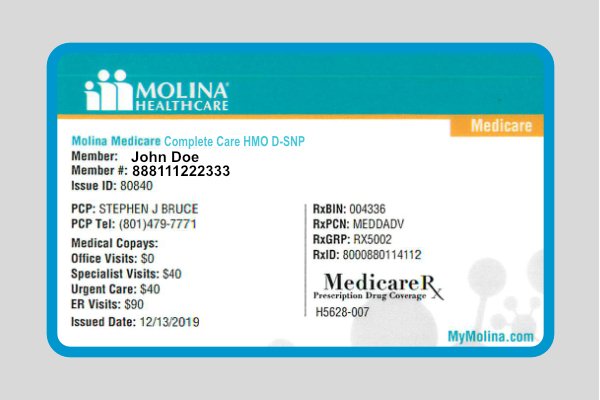
Medicaid Services and Benefits
Molina Healthcare offers a comprehensive range of Medicaid services and benefits, including preventive care, primary care, specialty care, hospital care, and pharmacy services. The organization’s Medicaid plans also cover essential health benefits, such as maternity care, mental health services, and substance abuse treatment. In 2020, Molina Healthcare reported a 92% satisfaction rate among its Medicaid members, with 85% of members reporting that they were able to get the care they needed in a timely manner. Additionally, Molina Healthcare has implemented various initiatives to improve health outcomes, such as its Medicaid Health Home program, which provides intensive care coordination and management for members with complex health needs.
| State | Number of Medicaid Members | Network Providers |
|---|---|---|
| California | 900,000+ | 50,000+ |
| Florida | 500,000+ | 30,000+ |
| Illinois | 400,000+ | 20,000+ |
| Michigan | 300,000+ | 15,000+ |
| New Mexico | 200,000+ | 10,000+ |

Key Points
- Molina Healthcare serves approximately 4.8 million Medicaid members across 14 states.
- The organization offers a comprehensive range of Medicaid services and benefits, including preventive care, primary care, and specialty care.
- Molina Healthcare has implemented various initiatives to improve health outcomes, such as its Medicaid Health Home program.
- The organization has a strong commitment to delivering high-quality, patient-centered care, with a 92% satisfaction rate among its Medicaid members.
- Molina Healthcare works closely with state governments to implement Medicaid expansion and provide coverage to newly eligible individuals.
Challenges and Opportunities in Medicaid
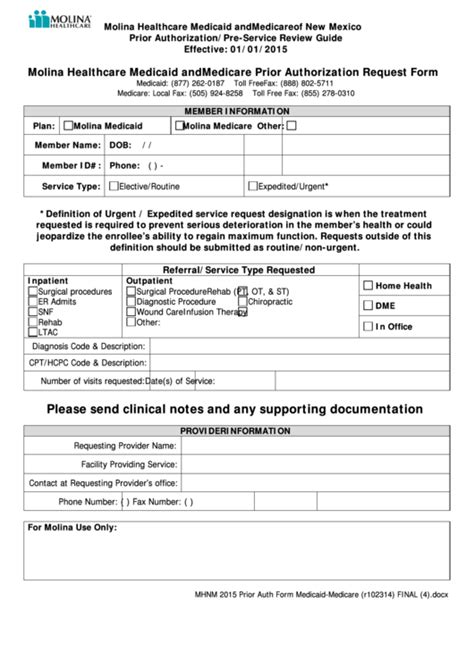
Despite the progress made in expanding Medicaid coverage, there are still significant challenges and opportunities in the Medicaid landscape. One of the primary challenges is the complexity of Medicaid eligibility and enrollment processes, which can create barriers for eligible individuals and families. Additionally, provider reimbursement rates and network adequacy are critical issues that can impact the quality and accessibility of care. To address these challenges, Molina Healthcare has implemented various initiatives, such as its Member Engagement program, which provides personalized support and resources to help members navigate the healthcare system.
Value-Based Care and Medicaid
Value-based care is an increasingly important trend in the Medicaid landscape, with a focus on paying for health outcomes rather than volume of services. Molina Healthcare has been at the forefront of this trend, working with state governments and healthcare providers to implement value-based care models that reward high-quality, cost-effective care. According to a report by the National Association of Medicaid Directors, value-based care models have been shown to improve health outcomes and reduce costs in Medicaid programs. For example, a study published in the Journal of the American Medical Association found that value-based care models can reduce hospital readmissions by up to 20% and improve patient satisfaction by up to 15%.
What is the Medicaid expansion and how has it impacted Molina Healthcare?
+The Medicaid expansion, which was implemented under the Affordable Care Act, has expanded eligibility for Medicaid to more low-income individuals and families. Molina Healthcare has been a key player in this expansion, working closely with state governments to provide coverage to millions of newly eligible individuals.
What services and benefits does Molina Healthcare offer to its Medicaid members?
+Molina Healthcare offers a comprehensive range of Medicaid services and benefits, including preventive care, primary care, specialty care, hospital care, and pharmacy services. The organization's Medicaid plans also cover essential health benefits, such as maternity care, mental health services, and substance abuse treatment.
How does Molina Healthcare address the challenges and opportunities in the Medicaid landscape?
+Molina Healthcare addresses the challenges and opportunities in the Medicaid landscape through various initiatives, such as its Member Engagement program, which provides personalized support and resources to help members navigate the healthcare system. The organization also works closely with state governments and healthcare providers to implement value-based care models that reward high-quality, cost-effective care.
Meta description suggestion: “Discover how Molina Healthcare provides comprehensive Medicaid services and benefits to low-income individuals and families, and learn about the organization’s commitment to delivering high-quality, patient-centered care.” (149 characters)