The MMR vaccine, which protects against measles, mumps, and rubella, is a crucial component of public health initiatives aimed at preventing the spread of these infectious diseases. However, concerns about the safety of vaccines during pregnancy have led to a significant amount of discussion and debate. It is essential to understand the risks and benefits associated with the MMR vaccine during pregnancy to make informed decisions about vaccination.
MMR Vaccine and Pregnancy: Understanding the Risks
The MMR vaccine is a live, attenuated vaccine, meaning it contains weakened forms of the measles, mumps, and rubella viruses. Live vaccines are generally not recommended during pregnancy due to the theoretical risk of transmission of the live, attenuated virus to the fetus. However, the risk of transmission and the potential consequences for the fetus are not well understood and are the subject of ongoing research.
Historical Context and Evolution of Recommendations
Historically, the recommendation has been to avoid live vaccines, including the MMR vaccine, during pregnancy as a precautionary measure. This recommendation is based on the theoretical risk of vaccine virus transmission to the fetus and the potential for congenital infection. However, the actual risk of such transmission and the consequences for the fetus are considered to be extremely low.
Studies and surveillance data have not identified a significant increase in the risk of congenital abnormalities or other adverse outcomes in infants born to mothers who received the MMR vaccine during pregnancy. The Advisory Committee on Immunization Practices (ACIP) and other health organizations have carefully considered these data in formulating guidelines for MMR vaccination during pregnancy.
| Category | Risk Assessment |
|---|---|
| Pregnancy | Generally not recommended due to theoretical risks, but benefits may outweigh risks in specific situations (e.g., outbreaks or travel to areas with high disease prevalence) |
| Breastfeeding | Considered safe; live vaccines, including MMR, do not affect the safety of breastfeeding |
| Immune Status | Individuals with weakened immune systems should avoid live vaccines, including MMR, due to increased risk of vaccine-related complications |

Benefits of MMR Vaccination

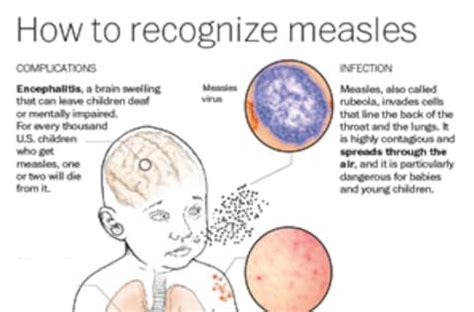
Despite the precautions regarding live vaccines during pregnancy, the benefits of MMR vaccination should not be underestimated. The vaccine is highly effective in preventing measles, mumps, and rubella, all of which can have serious complications, especially in non-immune individuals. In the context of pregnancy, preventing these diseases is crucial, as they can lead to severe outcomes for both the mother and the fetus.
Strategic Considerations for Vaccination
For women of childbearing age who are not pregnant, ensuring they are up to date with all recommended vaccinations, including MMR, is a critical preventive measure. This approach not only protects the individual but also contributes to herd immunity, reducing the risk of disease transmission in the community.
In situations where pregnancy is planned, women should discuss their vaccination status with their healthcare provider. If they are not immune to measles, mumps, or rubella, vaccination should be considered before conception, as live vaccines are generally not recommended during pregnancy.
Key Points
- The MMR vaccine is not recommended during pregnancy due to theoretical risks, but it may be considered in specific situations where the benefits outweigh the risks.
- Women of childbearing age should ensure they are up to date with all recommended vaccinations before becoming pregnant.
- The decision to vaccinate during pregnancy should be made on a case-by-case basis, considering individual risk factors and the potential benefits and risks of vaccination.
- Live vaccines, including MMR, are considered safe during breastfeeding.
- Individuals with weakened immune systems should avoid live vaccines due to increased risk of complications.
Addressing Concerns and Limitations
While the MMR vaccine is highly effective and safe for the general population, concerns about its use during pregnancy are valid and warrant careful consideration. The primary limitation of current knowledge is the lack of extensive data on the outcomes of pregnancies in which the MMR vaccine was administered. However, the available evidence and ongoing surveillance do not indicate a significant risk of adverse outcomes associated with MMR vaccination during pregnancy.
Healthcare providers play a crucial role in addressing these concerns and providing evidence-based guidance to pregnant women or those planning pregnancy. Open communication about the risks and benefits of vaccination, as well as the importance of preventing infectious diseases, is essential for informed decision-making.
Is the MMR vaccine safe during pregnancy?
+The MMR vaccine is generally not recommended during pregnancy due to theoretical risks of transmitting the live, attenuated virus to the fetus. However, the actual risk is considered to be extremely low, and the vaccine may be considered in specific situations where the benefits outweigh the risks.
Can I get the MMR vaccine while breastfeeding?
+Yes, the MMR vaccine is considered safe during breastfeeding. Live vaccines, including MMR, do not affect the safety of breastfeeding.
What are the benefits of MMR vaccination before pregnancy?
+Ensuring immunity to measles, mumps, and rubella before pregnancy can prevent these diseases during pregnancy, reducing the risk of severe outcomes for both the mother and the fetus. It also contributes to herd immunity, reducing the risk of disease transmission in the community.
In conclusion, while the MMR vaccine is not recommended during pregnancy due to theoretical risks, the benefits of vaccination in preventing measles, mumps, and rubella should not be overlooked. Healthcare providers and pregnant women or those planning pregnancy must weigh the potential risks and benefits of MMR vaccination on a case-by-case basis, considering individual risk factors and the context of disease prevalence and outbreaks. By doing so, informed decisions can be made to protect the health of both the mother and the fetus.



