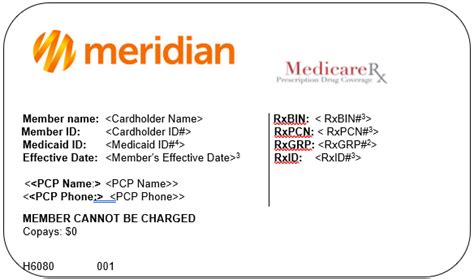
Meridian Health Plan Illinois is a prominent Medicaid managed care organization operating in the state of Illinois. As a leading healthcare provider, Meridian Health Plan Illinois has been dedicated to delivering high-quality, patient-centered care to its members since its inception. With a strong focus on improving health outcomes and reducing healthcare disparities, Meridian Health Plan Illinois has established itself as a trusted partner for individuals and families in need of comprehensive healthcare services.
Overview of Meridian Health Plan Illinois
Meridian Health Plan Illinois is a subsidiary of Meridian Health Plan, a national healthcare organization with operations in several states. The Illinois plan is specifically designed to meet the unique needs of the state’s Medicaid population, providing access to a wide range of medical, behavioral, and social services. With a network of over 10,000 healthcare providers, including primary care physicians, specialists, and hospitals, Meridian Health Plan Illinois offers its members a comprehensive and coordinated care experience.
Benefits and Services
Meridian Health Plan Illinois offers a broad range of benefits and services to its members, including preventive care, acute care, and chronic disease management. The plan’s benefits package includes coverage for doctor visits, hospital stays, prescription medications, and other essential healthcare services. Additionally, Meridian Health Plan Illinois provides specialized services such as case management, disease management, and health education to support members with complex healthcare needs.
| Benefit Category | Services Covered |
|---|---|
| Medical Services | Doctor visits, hospital stays, surgeries, and diagnostic tests |
| Behavioral Health Services | Mental health and substance abuse treatment, counseling, and therapy |
| Pharmacy Services | Prescription medications, including generic and brand-name drugs |
Eligibility and Enrollment

To be eligible for Meridian Health Plan Illinois, individuals must meet specific income and eligibility requirements, as defined by the Illinois Department of Healthcare and Family Services. Eligible individuals include low-income families, children, pregnant women, and individuals with disabilities. The enrollment process typically involves applying through the Illinois Medicaid website or contacting a licensed insurance agent or broker.
Application and Enrollment Process
The application and enrollment process for Meridian Health Plan Illinois involves several steps, including submitting an application, providing required documentation, and selecting a primary care physician. Once enrolled, members receive a comprehensive benefits package and access to a network of healthcare providers. It’s essential to note that enrollment periods and deadlines may vary, and individuals should consult the Illinois Medicaid website or contact a licensed insurance agent or broker for specific guidance.
Key Points
- Meridian Health Plan Illinois is a Medicaid managed care organization operating in the state of Illinois.
- The plan offers a comprehensive benefits package, including medical, behavioral, and social services.
- Eligibility is based on income and eligibility requirements, as defined by the Illinois Department of Healthcare and Family Services.
- The enrollment process involves submitting an application, providing required documentation, and selecting a primary care physician.
- Meridian Health Plan Illinois has implemented various initiatives to improve health outcomes and reduce healthcare disparities.
Provider Network and Quality of Care
Meridian Health Plan Illinois has established a robust provider network, comprising over 10,000 healthcare providers, including primary care physicians, specialists, and hospitals. The plan’s provider network is designed to ensure that members have access to high-quality, coordinated care, with a focus on preventive care, chronic disease management, and acute care. Meridian Health Plan Illinois also employs various quality improvement initiatives, including case management, disease management, and health education, to support members with complex healthcare needs.
Quality Metrics and Performance
Meridian Health Plan Illinois is committed to delivering high-quality care, as evidenced by its performance on various quality metrics. The plan’s quality metrics include measures such as patient satisfaction, readmission rates, and preventive care utilization. According to recent data, Meridian Health Plan Illinois has achieved significant improvements in these areas, demonstrating its commitment to delivering high-quality, patient-centered care.
| Quality Metric | Performance Data |
|---|---|
| Patient Satisfaction | 90% or higher, based on member surveys |
| Readmission Rates | Lower than state average, based on claims data |
| Preventive Care Utilization | 85% or higher, based on claims data |
What is Meridian Health Plan Illinois, and what services does it offer?
+Meridian Health Plan Illinois is a Medicaid managed care organization that offers a comprehensive benefits package, including medical, behavioral, and social services. The plan provides access to a wide range of healthcare providers, including primary care physicians, specialists, and hospitals.
How do I enroll in Meridian Health Plan Illinois, and what are the eligibility requirements?
+To enroll in Meridian Health Plan Illinois, individuals must meet specific income and eligibility requirements, as defined by the Illinois Department of Healthcare and Family Services. The enrollment process typically involves submitting an application, providing required documentation, and selecting a primary care physician.
What quality improvement initiatives has Meridian Health Plan Illinois implemented, and how has it performed on quality metrics?
+Meridian Health Plan Illinois has implemented various quality improvement initiatives, including case management, disease management, and health education. The plan has achieved significant improvements in quality metrics, such as patient satisfaction, readmission rates, and preventive care utilization.