Meningitis, a potentially life-threatening infection that inflames the membranes surrounding the brain and spinal cord, can strike at any age. The development and widespread use of meningitis vaccines have significantly reduced the incidence of this disease, particularly among young people. As a public health measure, vaccination against meningitis is crucial, and understanding the facts about these vaccines is essential for making informed decisions about health. Here, we delve into five key facts about meningitis vaccines, exploring their types, effectiveness, and the importance of vaccination in preventing meningitis outbreaks.
Types of Meningitis Vaccines

There are several types of meningitis vaccines, each designed to protect against different serogroups of the bacteria that cause meningitis. The primary types include MenACWY (which protects against serogroups A, C, W, and Y) and MenB (which protects against serogroup B). MenACWY vaccines are conjugate vaccines, meaning they link the weakened bacteria to a carrier protein to produce a stronger immune response. MenB vaccines, on the other hand, are not conjugate vaccines and work by directly introducing pieces of the outer membrane of the MenB bacteria to the body, prompting an immune response. Understanding the differences between these vaccines is crucial for determining the best protection strategy against meningitis.
Vaccine Effectiveness and Duration of Protection
Studies have shown that meningitis vaccines are highly effective in preventing invasive meningococcal disease (IMD). For instance, MenACWY vaccines have been demonstrated to provide protection against serogroups A, C, W, and Y for at least 5 years, with some studies suggesting longer protection. The effectiveness of MenB vaccines has also been documented, though the duration of protection may vary. Booster shots are often recommended to maintain immunity, especially for individuals at increased risk, such as those with certain medical conditions or attending college. The precise duration of protection and the need for booster shots can depend on the specific vaccine and individual factors, highlighting the importance of consulting healthcare professionals for personalized advice.
| Vaccine Type | Serogroups Protected Against | Typical Age of Administration |
|---|---|---|
| MenACWY | A, C, W, Y | 11-12 years, with a booster at 16 years |
| MenB | B | 16-18 years, or as recommended by a healthcare provider |

Key Considerations for Vaccination

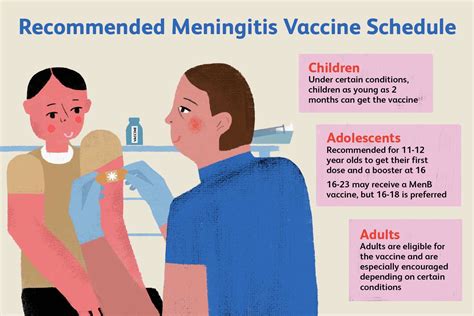
Vaccination against meningitis is particularly recommended for certain groups at higher risk, including adolescents, young adults, especially those living in close quarters like college dormitories, and individuals with certain immune system disorders. Additionally, travelers to areas with high rates of meningitis, such as the meningitis belt in Africa, should consider vaccination. The Centers for Disease Control and Prevention (CDC) and other global health authorities provide guidelines on who should receive meningitis vaccines, emphasizing the importance of consulting with a healthcare provider to determine the best vaccination strategy based on individual risk factors and health status.
Vaccine Safety and Side Effects
Like all vaccines, meningitis vaccines can cause side effects, though they are generally mild and temporary. Common side effects include redness, swelling, or pain at the injection site, and less frequently, fever or headache. Serious side effects are rare. The safety of meningitis vaccines is continuously monitored by health authorities, and the benefits of vaccination in preventing serious and potentially life-threatening disease far outweigh the risks associated with vaccine administration.
Key Points
- There are different types of meningitis vaccines, including MenACWY and MenB, each protecting against different serogroups of meningitis-causing bacteria.
- Meningitis vaccines are highly effective but not 100% effective, and booster shots may be necessary to maintain immunity.
- Certain groups, such as adolescents, young adults, and individuals with specific health conditions, are at higher risk and should prioritize vaccination.
- Vaccination is recommended for travelers to areas with high meningitis rates and for those living in close quarters, like college students.
- While side effects can occur, they are typically mild, and the vaccines are considered safe, with benefits outweighing risks.
FAQs on Meningitis Vaccines
What is the recommended age for meningitis vaccination?
+The recommended age for meningitis vaccination varies. Typically, the first dose of MenACWY is given at 11-12 years, with a booster dose at 16 years. MenB vaccination is recommended for adolescents aged 16-18 years, or as advised by a healthcare provider based on individual risk factors.
Are meningitis vaccines effective against all types of meningitis?
+No, meningitis vaccines protect against specific serogroups of Neisseria meningitidis, the bacteria most commonly causing meningitis. MenACWY vaccines protect against serogroups A, C, W, and Y, while MenB vaccines protect against serogroup B. Vaccination does not guarantee protection against all types of meningitis, especially those caused by other bacteria or viruses.
Can I get meningitis if I’ve been vaccinated?
+Yes, although rare, it is possible to contract meningitis even after being vaccinated. This can occur if the vaccine does not cover the specific serogroup causing the infection or if the individual’s immune response to the vaccine is not strong enough. It’s crucial to recognize the symptoms of meningitis and seek immediate medical attention if suspected.
In conclusion, meningitis vaccines represent a crucial tool in the prevention of meningococcal disease, offering significant protection against serious and potentially life-threatening infections. By understanding the types of vaccines available, their effectiveness, and the recommended vaccination schedules, individuals can make informed decisions about their health and the health of their loved ones. As with any medical intervention, consulting with a healthcare provider is essential for determining the most appropriate vaccination strategy based on individual risk factors and health status.