Hepatitis A is a highly contagious liver infection caused by the hepatitis A virus (HAV). It is primarily spread through the fecal-oral route, where the virus is ingested through contaminated food, water, or direct contact with an infected person. The hepatitis A vaccine has been a crucial tool in preventing the spread of the disease, and its impact has been significant. In this article, we will explore five ways the hepatitis A vaccine has made a difference in public health.
Key Points
- The hepatitis A vaccine has been shown to be highly effective in preventing the disease, with a success rate of over 95% after two doses.
- Widespread vaccination has led to a significant decline in hepatitis A cases, with a reported 92% decrease in the United States between 1995 and 2011.
- The vaccine has been particularly beneficial for high-risk groups, such as travelers to areas with high hepatitis A endemicity, men who have sex with men, and individuals with liver disease.
- Implementation of hepatitis A vaccination programs in schools and childcare settings has helped to prevent outbreaks and reduce the spread of the disease.
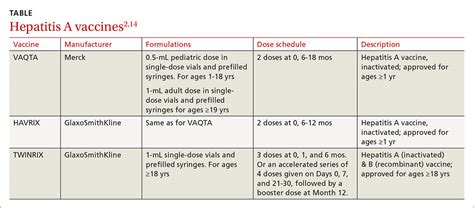
- Ongoing research and development of new vaccine formulations, such as combination vaccines, aim to further improve protection and simplify vaccination schedules.
Effectiveness of the Hepatitis A Vaccine
The hepatitis A vaccine has undergone extensive testing and has been proven to be highly effective in preventing the disease. According to the Centers for Disease Control and Prevention (CDC), the vaccine is over 95% effective in preventing hepatitis A after two doses. This high efficacy rate is attributed to the vaccine’s ability to stimulate the production of antibodies, which provide long-term protection against the virus. Studies have consistently shown that the vaccine is safe and well-tolerated, with common side effects being mild and temporary.
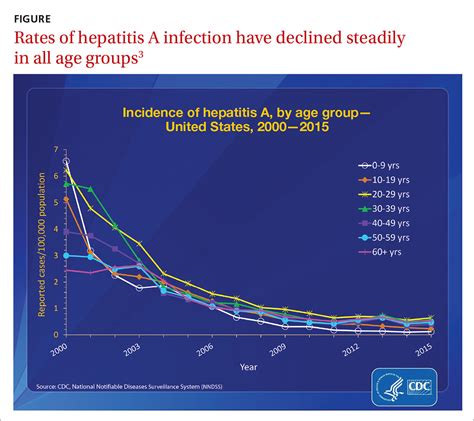
Decline in Hepatitis A Cases
The introduction of the hepatitis A vaccine has led to a significant decline in hepatitis A cases worldwide. In the United States, for example, the CDC reported a 92% decrease in hepatitis A cases between 1995 and 2011. This decline is largely attributed to the widespread adoption of hepatitis A vaccination programs, particularly among high-risk groups. Targeted vaccination efforts have been instrumental in reducing the spread of the disease, and continued vaccination is essential to maintaining low case rates.
| Year | Hepatitis A Cases (United States) |
|---|---|
| 1995 | 31,032 |
| 2001 | 10,659 |
| 2011 | 2,529 |
Benefits for High-Risk Groups
The hepatitis A vaccine has been particularly beneficial for high-risk groups, such as travelers to areas with high hepatitis A endemicity, men who have sex with men, and individuals with liver disease. These groups are at increased risk of contracting the disease due to various factors, including exposure to contaminated food and water, sexual practices, and underlying health conditions. Vaccination is essential for these groups, as it provides protection against the disease and reduces the risk of complications and transmission to others.
Vaccination Programs in Schools and Childcare Settings
Implementation of hepatitis A vaccination programs in schools and childcare settings has helped to prevent outbreaks and reduce the spread of the disease. These programs aim to vaccinate children and staff, particularly in areas with high hepatitis A endemicity, to prevent the spread of the disease. Early vaccination is crucial in preventing the spread of the disease, as children are often asymptomatic carriers of the virus and can transmit it to others.
Ongoing Research and Development
Ongoing research and development of new vaccine formulations, such as combination vaccines, aim to further improve protection and simplify vaccination schedules. Combination vaccines, which combine multiple vaccines into a single dose, have the potential to reduce the number of injections required and improve vaccine compliance. Researchers are also exploring new vaccine technologies, such as mRNA vaccines, which may offer improved efficacy and safety profiles.
What is the recommended schedule for hepatitis A vaccination?
+The recommended schedule for hepatitis A vaccination is two doses, given 6-12 months apart. The first dose is typically given at 12-23 months of age, and the second dose is given 6-12 months later.
Who is at high risk for hepatitis A?
+High-risk groups for hepatitis A include travelers to areas with high hepatitis A endemicity, men who have sex with men, individuals with liver disease, and people who use illicit drugs.
Can hepatitis A be prevented through good hygiene practices?
+Good hygiene practices, such as frequent handwashing and proper food handling, can help reduce the risk of hepatitis A transmission. However, vaccination is the most effective way to prevent the disease.
In conclusion, the hepatitis A vaccine has made a significant impact on public health by preventing the spread of the disease and reducing the number of cases and outbreaks. Its effectiveness, benefits for high-risk groups, and implementation in schools and childcare settings have all contributed to its success. Ongoing research and development of new vaccine formulations will continue to improve protection and simplify vaccination schedules, ensuring that the hepatitis A vaccine remains a crucial tool in the prevention of this highly contagious liver infection.