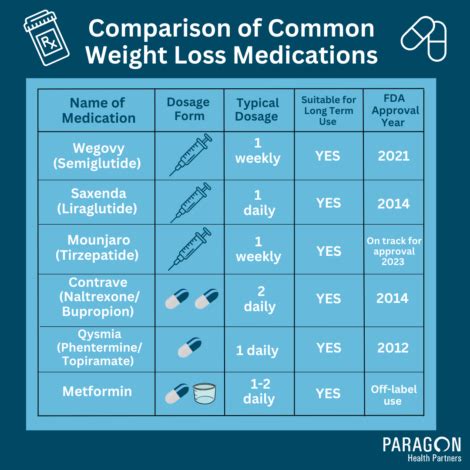
United Healthcare, one of the largest health insurance providers in the United States, offers a wide range of coverage options for various medical treatments and medications. Wegovy, a brand name for the medication semaglutide, is a prescription drug used for chronic weight management in adults with obesity or overweight with at least one weight-related condition. The coverage for Wegovy under United Healthcare plans can vary depending on several factors, including the specific plan type, the state where the policy is issued, and the individual's medical history and needs.
Understanding United Healthcare’s Coverage Policy

Generally, United Healthcare covers medications that are approved by the U.S. Food and Drug Administration (FDA) for specific indications. Since Wegovy is FDA-approved for chronic weight management, it is potentially covered under many United Healthcare plans. However, the extent of coverage, including copays, coinsurance, and deductibles, can differ significantly between plans.
Factors Influencing Coverage
Several factors can influence whether and how United Healthcare covers Wegovy for an individual. These include:
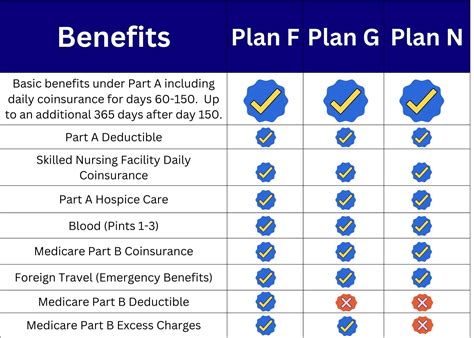
- Plan Type: Different types of plans (e.g., HMO, PPO, Medicare Advantage) may have varying levels of coverage for prescription medications like Wegovy.
- Formulary Status: United Healthcare maintains a formulary, which is a list of prescription drugs that are covered by the plan. The status of Wegovy on this formulary can affect its coverage.
- Prior Authorization: Some plans may require prior authorization from a healthcare provider before covering Wegovy, to ensure it is prescribed for a covered indication and that other criteria are met.
- Step Therapy: In some cases, insurance plans may require trying other weight loss treatments before approving coverage for Wegovy.
| Plan Feature | Impact on Coverage |
|---|---|
| Formulary Tier | Placement on a higher tier can increase out-of-pocket costs for the patient. |
| Prior Authorization Requirements | May delay access to Wegovy until approval is obtained. |
| Step Therapy Requirements | Can delay treatment with Wegovy until other treatments have been tried. |
Appealing Coverage Decisions
If United Healthcare denies coverage for Wegovy, individuals have the right to appeal the decision. This process typically involves submitting additional information from a healthcare provider to support the medical necessity of the treatment. Understanding the appeals process and the criteria used by United Healthcare to make coverage decisions can be crucial in obtaining coverage for necessary medications like Wegovy.
Key Points
- United Healthcare's coverage of Wegovy varies by plan and individual circumstances.
- Formulary status, prior authorization, and step therapy requirements can influence coverage.
- Reviewing plan documents and consulting with insurance representatives is essential for understanding coverage details.
- Appeals processes are available for denied coverage decisions.
- Healthcare providers play a critical role in supporting coverage by providing medical necessity documentation.
Given the complexity of health insurance coverage and the specifics of individual plans, it's crucial for those seeking coverage for Wegovy under United Healthcare to navigate their plan's details carefully and to seek professional advice when needed. Staying informed about coverage policies and advocating for necessary treatments can make a significant difference in accessing effective care for chronic weight management.
How do I find out if my United Healthcare plan covers Wegovy?
+To determine if your United Healthcare plan covers Wegovy, you should review your plan documents, visit the United Healthcare website, or contact their customer service directly. They can provide you with the most current and detailed information regarding the coverage of Wegovy under your specific plan.
What if my United Healthcare plan denies coverage for Wegovy?
+If your United Healthcare plan denies coverage for Wegovy, you have the right to appeal the decision. This typically involves working with your healthcare provider to submit an appeal, providing additional information that supports the medical necessity of Wegovy for your condition. Understanding the appeals process and the criteria used by United Healthcare can help in making a strong case for coverage.